Tuberculosis (TB) of extra-pulmonary tissues is most often a spread of infection via the blood stream from a primary lung focus. It sets up a chronic granulomatous infection in the bone and/orjoint.
Aetiology/Pathogenesis
Skeletal TB is caused by Mycobacterium tuberculosis. Atypical cases caused by other Mycobacterial species are discussed below. In past times, M. bovis caused a lot of skeletal TB by haematogenous spread from the GIT (from drinking infected milk); this is now rare after the introduction of pasteurisation.
Haematogenous seeding of tuberculous bacilli is the most common form of skeletal infection. Occasionally direct extension from adjacent foci (lung, kidney, lymph nodes) is seen. Direct traumatic inoculation is more the cause for non-tuberculous Mycobacterial infection (see below).
Pathology
Like TB elsewhere, bone and joint react to infection by forming granulomas. Central caseating necrosis surrounded by multinucleate-giant cells and epithelioid cells and lymphocytes at the periphery are observed. The joint synovium becomes inflamed and forms a pannus of granulation tissue which erodes into the cartilage and bone. Unlike pyogenic infections, chronic granulomatous infection takes a long time to reduce the joint space.
TB Spondylitis (Pott's disease)
Initially described by Sir Percival Pott in 1779, the spine accounts for - 50% of skeletal TB, most commonly affecting vertebrae T8 to L3. Patients complain of back pain, and signs include:
· bony tenderness
· kyphos (swelling over the area of infection)
· kyphosis/scoliosis
· nerve root compression
· signs of paralysis
Disease begins in the anterior vertebral body. The adjacent disc becomes involved, leading to narrowing of disc space and herniation. Eventually the vertebra collapses and anterior wedging occurs leading to kyphosis and/or scoliosis. The posterior vertebral structures (pedicle, spine) are rarely involved. Cold (i.e. not inflamed) abscesses are formed adjacent to the vertebral column, and calcification of the cavity is pathognomonic for TB. Clinically pyogenic and tuberculous spondylitis cannot be distinguished. Diagnosis must be made microbiologically.
Radiology and/or CT scan of Pott's disease shows:
· narrowed disc space
· kyphoscoliosis
· soft tissue swelling
· cold abscesses (may be calcified) · bony erosion (scalloping)
TB Osteomyelitis
Haematogenously-spread TB affects the metaphysis, commonly femur and tibia, and the small bones of the hands and feet. Elderly patients have been reported to present with TB in tarsal/metatarsal bones.
On X-ray, the osteolytic lesions appear identical to those caused by pyogenic bacteria. However metaphyseal TB spreads across the physis (transphyseal spread) whereas pyogenic infections do not. Tuberculous dactylics is more common in children and has characteristic appearances:
· soft tissue swelling of multiple digits
· lytic lesions of several metacarpals/prox. phalanges
· gross periostitis.
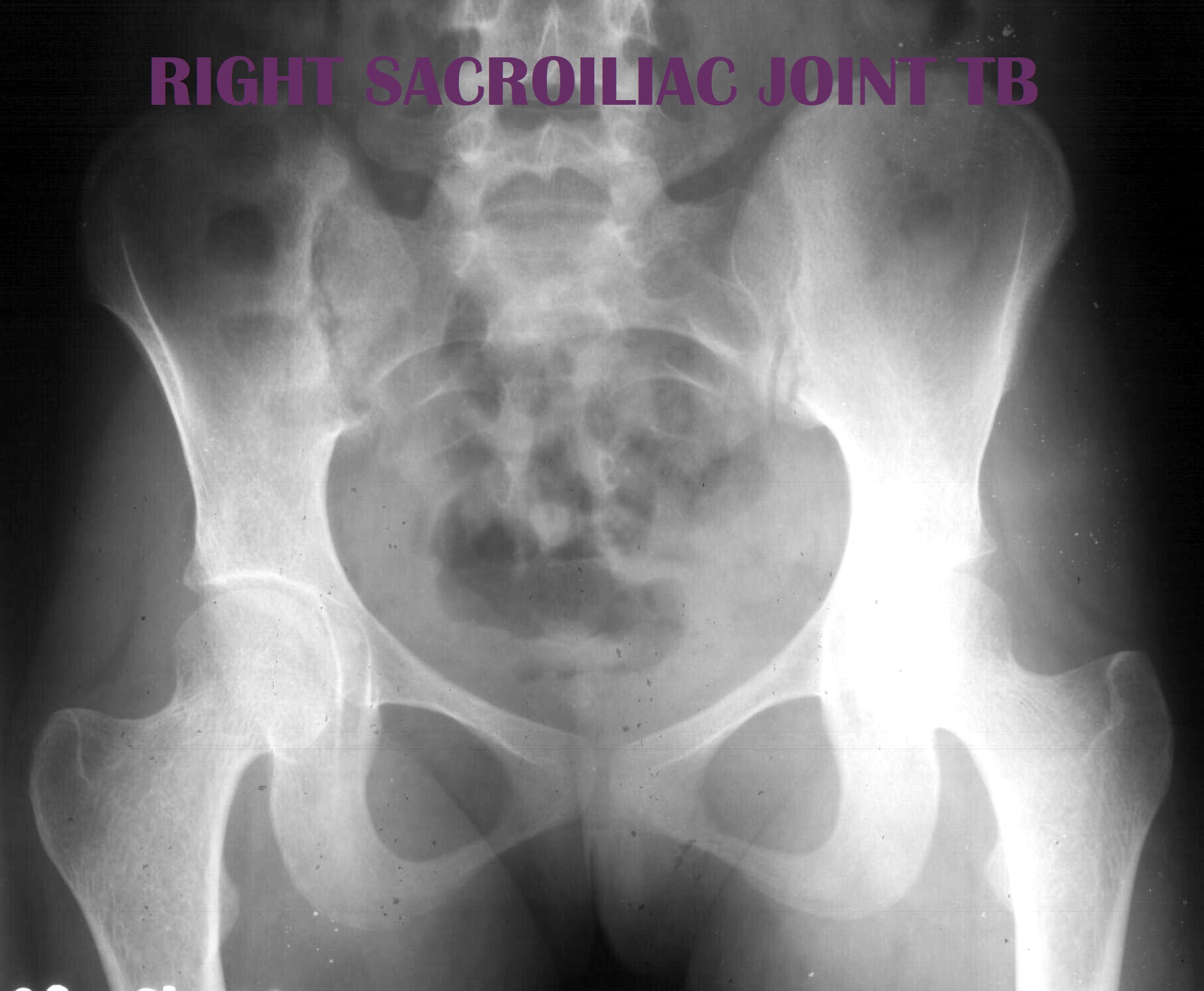
TB Arthritis
Characteristically, a monoarticular infection of weight-bearing joints (hip, knee). Symptoms of pain and swelling are of insidious onset. Disease progression is so slow that it can be easily missed in the early stages. On X-ray, a triad of changes signals TB:
Phemister's triad:
· gradual narrowing ofjoint space
· subchondral osteoporosis
· peripherally-located osseous erosions