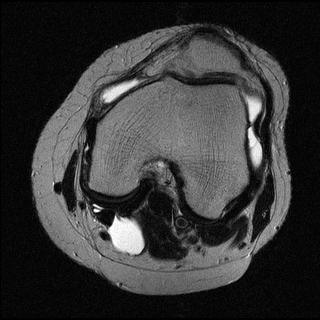
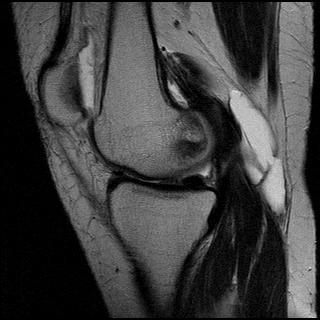
Early osteoarthritis with ruptured Bakers cyst.
The images show loss of articular cartilage along the inferior articulating surface of the medial femoral condyle .There is mild joint effusion with fluid in the suprapatellar bursa. A Bakers cyst x 1.7 x 1.6 is observed in the popliteal fossa. The inferior end of the cyst has ruptured and fluid is observed tracking along the proximal medial head of gastrocnemius .
Popliteal or Baker's cyst represents fluid distention of a bursa between the gastrocnemius and semimembranosus tendons via a communication with the knee joint .Although called the gastrocnemiosemimembranosus bursa, it represents a composite of two bursae: a bursa anterior to the medial gastrocnemius tendon (the subgastrocnemius bursa) and a bursa between the tendons of the gastrocnemius and semimembranosus tendons. Frequency of Baker's cysts identified on MR imaging ranges from 10% to 41%. Baker's cysts may be seen with many joint abnormalities, such as internal derangement, osteoarthrosis, or inflammatory arthritis; the most common associations include joint effusion, meniscal tear, and degenerative joint disease. Arthritis is the most common condition associated with Baker cyst. Of the arthritides, osteoarthritis is probably the most common cause of popliteal cyst. Although prevalence of Baker cyst in patients with inflammatory arthritis is higher than in patients with osteoarthritis, osteoarthritis is much more common than inflammatory arthritis.
The diagnosis of Baker's cyst is effectively made with MR imaging because fluid distention of the gastrocnemiosemimembranosus bursa is well depicted on T2-weighted axial MR images
The most common complication of Baker cyst is the rupture or dissection of fluid into the adjacent proximal gastrocnemius muscle belly, which results in a pseudothrombophlebitis syndrome mimicking symptoms of DVT.
Cysts Associated with the Knee Joint
1. Intraarticular Ganglion : Ganglia are cystic structures lined by flat spindle-shaped cells and contain mucin or fluid. Ganglia may arise from joint capsules, ligaments, tendon sheaths, bursae, or subchondral bone, and they generally do not communicate directly with the joint. In the knee, most ganglia arise near a cruciate ligament; the tibial end of the anterior cruciate ligament was the most common site of origin found in a recent arthroscopic series. On MR images, such a ganglion usually appears as a septated ovoid fluid collection adjacent to a cruciate ligament; bone erosion of the femoral condyle or extensive dissection along tissue planes may occur. Ganglia can be differentiated from meniscal cysts by the absence of connection to a meniscal tear, and they tend to be more septated than meniscal cysts.
2. Meniscal Cysts : Meniscal cysts are formed by extrusion of joint fluid through a meniscal tear into the adjacent tissues; thus, they indicate the presence of a meniscal tear . On MR images, lateral meniscal cysts appear as well-defined rounded cysts located adjacent to a meniscal tear. Lateral meniscal cysts are three to four times more common than medial meniscal cysts. Medial meniscal cysts tend to be larger and often dissect away from the site of meniscal tear, as the attachment of the peripheral edge of the meniscus to the medial collateral ligament prevents accumulation of fluid immediately adjacent to the meniscus.
3.Popliteal (Baker’s) Cysts : Popliteal cysts are lined with synovium and result from extrusion of joint fluid into the gastrocnemiosemimembranosus bursa through a weak portion of the posteromedial capsule - of the knee between the medial head of the gastrocnemius muscle and the semimembranosus muscle. This consistent anatomic feature helps differentiate popliteal cysts from other cystic masses in the popliteal region.
4.Intraosseous Cysts :Juxta-articular, intraosseous cysts may arise at the site of insertion of the cruciate ligaments or meniscotibial attachments and appear on MR images as small well-defined lesions with minimal or no edema in the adjacent marrow. Their origin is controversial, but they most likely result from bone resorption associated with chronic avulsive stress.
Bursae Around the Knee
1. Anserine bursitis :The anserine bursa separates the pes anserinus, which is formed by the distal parts of the tendons of the sartonus, gracihis, and semitendinosus muscles, from the subjacent distal portion of the tibial collateral ligament and the bony surface of the medial tibial condyle. On MR images, a fluid collection that does not communicate with the knee joint is seen adjacent to the pes anserinus.
2.Prepatellar Bursitis : The prepatellar bursa is located between the patella and the overlying subcutaneous tissues. Inflammatory and hemorrhagic bursitis result from chronic trauma, often due to occupational
or recreational kneeling and crawling (e.g., house-maid’s knee, carpet-layer’s knee). On MR images, prepatellar bursitis appears as a focal fluid collection between the patellar tendon and the subcutaneous tissues ,and it is often heterogeneous in signal intensity and poorly defined because of inflammation and hemorrhage.
3.Superficial Infrapatellar Bursitis : The superficial infrapatellar bursa is located between the tibial tubercle and the overlying skin. MR imaging shows a focal, poorly defined collection of fluid anterior to the tibial tubercle.
4.Deep Infrapatellar Bursitis :The deep infrapatellar bursa is located between the posterior margin of the distal part of the patellar tendon and the anterior aspect of the tibia. A tiny amount of fluid is occasionally seen in this location in asymptomatic patients.
5.Iliotibial Bursitis and Tendinitis : The iliotibial bursa is located between the distal part of the iliotibial band near its insertion on Gerdy’s tubercle and the adjacent tibial surface. MR images show a well-defined fluid collection near the insertion of the distal part of the iliotibial tendon onto the anterolateral surface of the tibia . Iliotibial tendonitis has similar clinical features; however, the MR findings of poorly defined increased signal within the tendon on T1– and T2-weighted images allow it to be differentiated from bursitis.
6.Tibial Collateral Ligament Bursitis :The tibial collateral ligament bursa is located between the superficial and deep layers of the medial collateral ligament. Bursitis in this location causes medial joint pain suggestive of injury of the medial meniscus or medial collateral ligament. MR images show a well-defined fluid collection between the deep and superficial portions of the medial collateral ligament. This condition must be differentiated from medial meniscal cysts or meniscocapsular separation. It is therefore important to rule out medial meniscal tear and to scrutinize the peripheral margin of the meniscus on T2- or T2*weighted coronal images.
Lesions That Mimic Cysts
1.Synovial Chondromatosis :Synovial osteochondromatosis is a chondroid metaplasia of the synovium that generates cartilaginous masses within the joint. These chondroid bodies may detach from the synovium and grow independently in the synovial fluid. On MR images, synovial osteochondromatosis usually is manifested by multiple low-signal-intensity nodules, occasionally containing high-signal-intensity marrow fat and associated with a variable amount of nodular synovial thickening. Uncalcified synovial chondromatosis can mimic an intraarticular cyst or loculated joint effusion on MR images, because the signal behavior of the metaplastic cartilage is dominated by its content of freely mobile water protons . Diagnosis of such cases relies on recognition of the highly nodular and lobulated configuration of the lesion on MR images.
2.Popliteal Vein Varix :Focal dilatation of the popliteal vein occasionally results from trauma of the vessel wall. Complications of varices of the popliteal vein include rupture, thrombosis, and embolism. The MR imaging appearance is nonspecific for a cyst ; however, identification of the connection with the popliteal vein allows a correct diagnosis. Saccular aneurysms of the popliteal artery may also mimic cysts in the popliteal fossa.