Introduction- Tumefactive demyelinating lesions are generally thought of as solitary lesions, greater than 2 cm, with imaging characteristics mimicking neoplasms. These lesions more commonly occur in women with an average age of 37 years .With rare exception, the tumefactive demyelinating lesions do not originate as a postinfectious or post-vaccination response.
Pathology-tumefactive demyelinating lesions represent an intermediate lesion between those typically seen with multiple sclerosis and acute disseminated encephalomyelitis. Pathologically, these lesions are indistinguishable from typical multiple sclerosis plaques and are characterized by infiltrating foamy macrophages intermingled between reactive astrocytes . Significant quantities of lipid may accumulate within the plaques as a result of myelin breakdown. The axons are relatively preserved within the lesions, but more recent investigation has shown axonal jury within multiple sclerosis plaques. The pathologic diagnosis may be challenging based on the initial frozen-section specimen when the primary suspicion is malignancy.
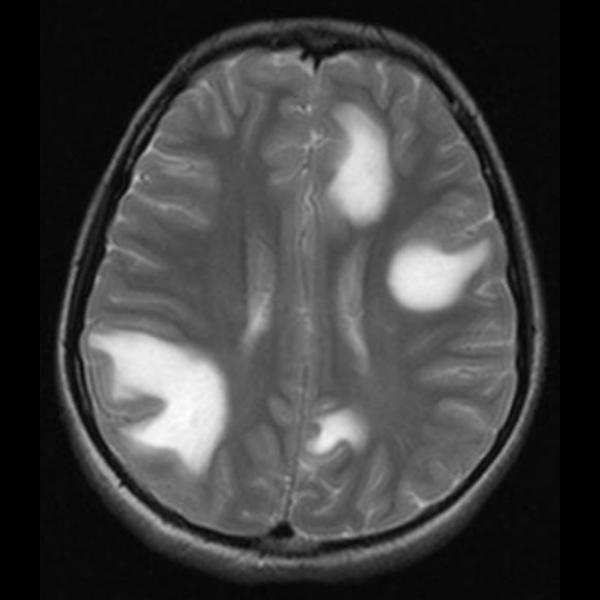
Imaging Features Suggestive of Tumefactive Demyelinating Lesions
a) Large Lesion with Little Mass Effect and Edema
Tumefactive demyelinating lesions tend to be circumscribed lesions with little mass effect or vasogenic edema. They typically involve the supratentorial compartment and are centered within the white matter, although they may extend to involve the cortical gray matter
b) Ringlike or Open-Ring Enhancement
Commonly the enhancement patterns will be in the form of an open ring, with the incomplete portion of the ring on the gray matter side of the lesion . More typical active multiple sclerosis plaques exhibit this open-ring or arclike pattern of enhancement only 9% of the time. The enhancing portion of the ring is believed to represent the leading edge of demyelination and thus favors the white matter side of the lesion. The central nonenhancing core represents a more chronic phase of the inflammatory process
c) Central Dilated Veins Within the Lesion
Cha et al. noted a dilated vascular structure running centrally within several of the studied tumefactive demyelinating lesions on T2 echoplanar images from MRI perfusion studies. These vascular structures were believed to represent dilated veins draining toward distended subependymal veins
d) Proton Spectroscopy
The area of enhancement reveals elevated choline (Cho) and suppressed N-acetylaspartate (NAA) relative to creatine (Cr) and prominent lactate (Lac) doublet.
e) Decreased Perfusion
Cha et al. reported the mean relative cerebral blood volume (rCBV) within tumefactive demyelinating lesions was lower than that within the contralateral normal-appearing white matter and substantially less than that found in high-grade gliomas and lymphomas.
f) Rapid Resolution After Steroid Therapy
Most tumefactive demyelinating lesions will show an excellent response to corticosteroid therapy with a substantial decrease in size or disappearance of the lesions on follow-up imaging
Most tumefactive demyelinating lesions will show an excellent response to corticosteroid therapy with a substantial decrease in size or disappearance of the lesions on follow-up imaging
Imaging Features Not Specific for Tumefactive Demyelinating Lesions
a) Corpus Callosum Involvement
Tumefactive demyelinating lesions can spread through or originate within the corpus callosum . As such, they should be listed in the differential diagnosis of \"butterfly\" lesions, with glioblastoma multiforme and lymphoma
Tumefactive demyelinating lesions can spread through or originate within the corpus callosum . As such, they should be listed in the differential diagnosis of \"butterfly\" lesions, with glioblastoma multiforme and lymphoma
b) Increased Diffusion
Diffusion imaging reveals mildly increased apparent diffusion coefficients within tumefactive demyelinating lesions .This proves to be a useful tool in differentiating ring-enhancing tumefactive demyelinating lesions from cerebral abscesses, the latter being associated with restricted diffusion centrally within the lesion. Necrotic neoplasms may display a similar increase in diffusion coefficients centrally within the lesion, making diffusion less helpful in differentiating from neoplasms
Diffusion imaging reveals mildly increased apparent diffusion coefficients within tumefactive demyelinating lesions .This proves to be a useful tool in differentiating ring-enhancing tumefactive demyelinating lesions from cerebral abscesses, the latter being associated with restricted diffusion centrally within the lesion. Necrotic neoplasms may display a similar increase in diffusion coefficients centrally within the lesion, making diffusion less helpful in differentiating from neoplasms
c) Tumorlike Spectrum on Proton MR Spectroscopy
Primary glial cell tumors produce a characteristic spectrum consisting of elevated choline with suppressed levels of N-acetylaspartate. Additionally, there may be detectable levels of lipids and lactate corresponding to necrosis and anaerobic metabolism associated with the glial tumors (primarily glioblastoma multiforme). Several nonneoplastic brain lesions (including tumefactive demyelinating lesions) may produce an identicalMR spectrum, mimicking a neoplastic process
Primary glial cell tumors produce a characteristic spectrum consisting of elevated choline with suppressed levels of N-acetylaspartate. Additionally, there may be detectable levels of lipids and lactate corresponding to necrosis and anaerobic metabolism associated with the glial tumors (primarily glioblastoma multiforme). Several nonneoplastic brain lesions (including tumefactive demyelinating lesions) may produce an identicalMR spectrum, mimicking a neoplastic process